Understanding LPP Hair Loss: Causes and Solutions

LPP Hair Loss: Understanding Causes and Effective Solutions

Lichen Planopilaris, a rare but serious skin condition that affects hair follicles, can be a source of distress for those affected by it. It is important to understand what causes this condition and how it can be treated. In this blog, we take a deep dive into understanding Lichen Planopilaris- its definition, prevalence, symptoms, and diagnosis process. We will also discuss the potential triggers and risk factors associated with the condition. Additionally, we will cover the course of treatment available to manage Lichen Planopilaris - both pharmacological and non-pharmacological measures. Lastly, we will talk about living with this condition and its prognosis. Read on to gain comprehensive insights into Lichen Planopilaris and how you can manage it effectively.
What is Lichen Planopilaris
Lichen planopilaris is a scarring hair loss condition characterized by inflammation and damage to the hair follicles. If left untreated, it can lead to permanent hair loss. Dermatologists diagnose lichen planopilaris through a biopsy. Treatment options for this condition focus on reducing inflammation and promoting hair regrowth. By using topical corticosteroids, dermatologists aim to improve the efficacy of treatment. Lichen planopilaris presents with symptoms of an itchy rash and may be associated with conditions like rheumatoid arthritis. (
Lichen planopilaris, a form of lichen planus that primarily affects the scalp, is an autoimmune disease where the immune system mistakenly targets the hair follicles. This condition can lead to hair loss and scarring on the scalp. Common symptoms include redness, itching, and irritation in the affected areas. Early diagnosis and treatment are key to effectively managing lichen planopilaris. It is essential to understand the characteristics of this condition for proper identification and timely intervention. Dermatology research and the Journal of the American Academy of Dermatology (JAAD) often provide insights into the efficacy of topical corticosteroids and other treatment options. Recognizing the symptoms of lichen planus and understanding its follicular variant, known as follicular lichen planus or lPP, can facilitate appropriate diagnosis and management. Additionally, it's important to note that individuals with lichen planopilaris may have an increased risk of developing rheumatoid arthritis.
Lichen planopilaris, a rare condition, affects both men and women, with a higher prevalence in middle-aged individuals. Factors like family history and autoimmune disorders can increase the risk. While the exact prevalence is unknown, it is estimated to affect less than 1% of the population. The impact on quality of life and self-esteem can be significant due to its symptoms and clinical features. Dermatology professionals often use topical corticosteroids for treatment, which have shown efficacy in managing this itchy rash.
The exact cause of lichen planopilaris remains unknown, but it is believed to be an autoimmune condition. Triggers such as stress, hormonal changes, and infections may contribute to its development. Those with a family history of lichen planopilaris or other autoimmune disorders may be at a higher risk. Genetic factors are also thought to play a role, although further research is needed for a full understanding of the causes and risk factors of this condition.
Who Gets Lichen Planopilaris
Lichen planopilaris predominantly affects young adult women, but it can occur across a wide demographic spectrum including men and individuals of various ages. The susceptibility to this condition appears to peak in middle-aged females, particularly those with a history of lichen planus affecting other areas of the body, such as the skin or mucous membranes. While the exact demographics remain unclear, research indicates that individuals with a family history of autoimmune disorders may be at a heightened risk.
The incidence of lichen planopilaris is relatively low, impacting less than 1% of the general population. However, due to its association with other autoimmune conditions, those with specific genetic backgrounds may find themselves more vulnerable. Understanding who is at risk can assist in early detection and intervention, ultimately improving management strategies and outcomes for those affected.
Causes of Lichen Planopilaris
The precise causes of lichen planopilaris remain elusive, but it is believed to stem from an autoimmune response wherein the immune system mistakenly targets hair follicles. Genetic factors play a minimal role, with the condition seldom presenting as hereditary. Environmental triggers such as certain medications or infections can also contribute to the onset of this disorder.
Moreover, stress and hormonal fluctuations have been recorded as potential triggers that may exacerbate existing cases of lichen planopilaris. Identifying these causes and triggers is crucial, as management strategies often focus on mitigating their effects to prevent disease progression. Understanding the underlying mechanisms of lichen planopilaris can pave the way for effective treatment plans tailored to individual needs.
Stress and Emotional Trauma and Flare-ups
Stress and emotional trauma have been associated with triggering flare-ups of lichen planopilaris. Hormonal changes, such as those experienced during menopause, can also contribute to the development of this condition. Infections caused by certain bacteria or viruses have also been linked to lichen planopilaris. Additionally, exposure to certain medications or chemicals can sometimes trigger the condition in susceptible individuals. It is important to identify and avoid potential triggers in order to effectively manage lichen planopilaris.
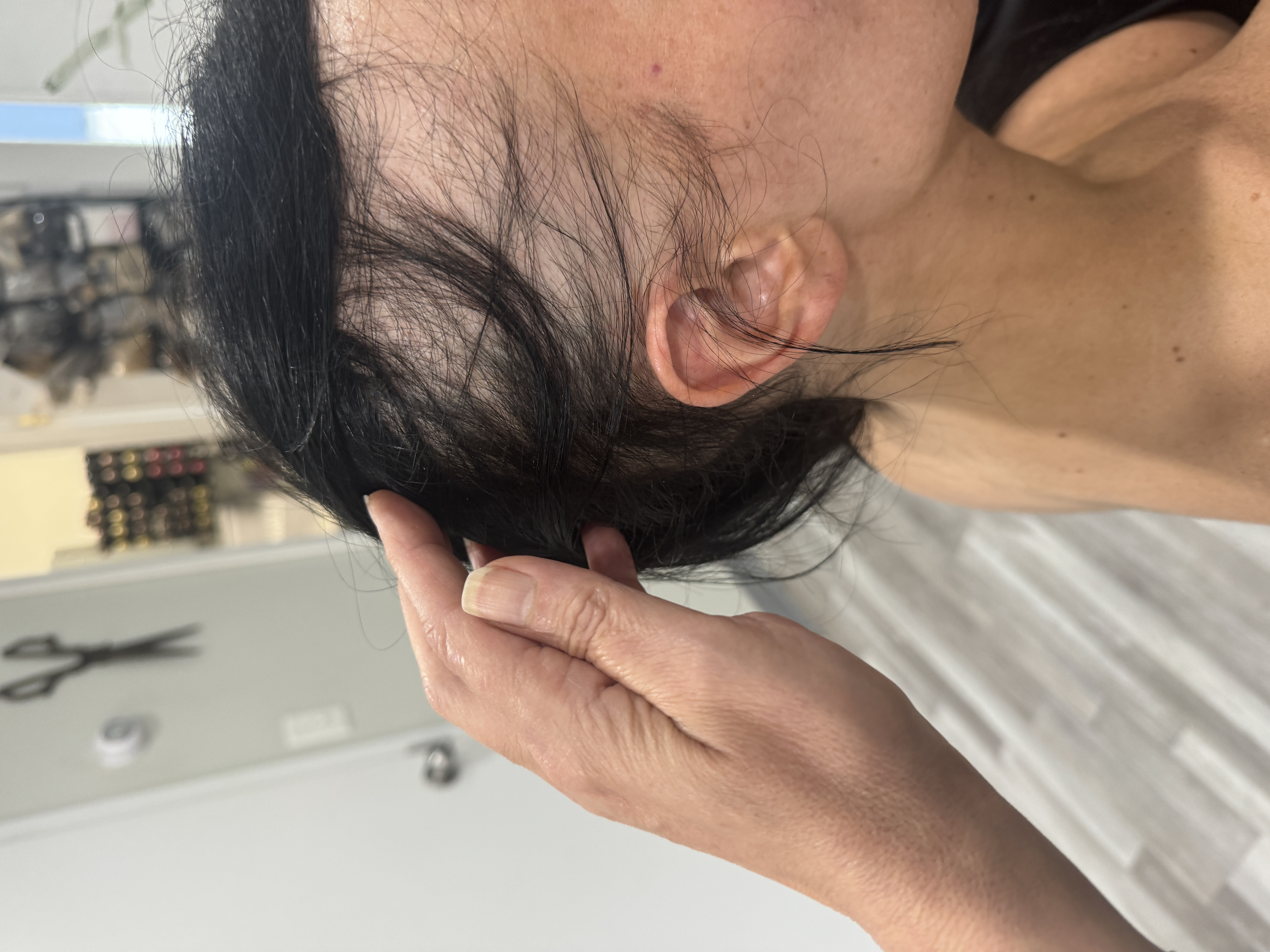
Lichen planopilaris, a dermatological condition, is characterized by specific symptoms and clinical features. Individuals with this condition often experience itching, redness, and irritation on their scalp. Hair loss is a prominent feature, leading to the development of bald patches. In severe cases, lichen planopilaris can cause scarring and permanent hair loss. Recognizing these symptoms is crucial as early diagnosis and treatment are essential. Seeking medical attention promptly can help manage the condition effectively.
Recognizing the Symptoms of Lichen Planopilaris can help in early diagnosis and treatment. Common symptoms include itching, burning, and tenderness on the scalp. Red or purple-colored bumps may appear, leading to hair loss. The affected areas may have a rough texture and scaly appearance, with swollen and inflamed hair follicles. If you experience these symptoms, it is recommended to consult with a dermatologist for proper evaluation and treatment.
Understanding the clinical features of lichen planopilaris is crucial for accurate diagnosis and appropriate treatment. In the early stages of the condition, individuals may experience redness, scaling, and small areas of hair loss on the scalp. As lichen planopilaris progresses, it can lead to larger bald patches and scarring. It's important to note that in some cases, lichen planopilaris may extend beyond the scalp, affecting other parts of the body. Recognizing these clinical features can help healthcare professionals provide effective management and care for patients with lichen planopilaris.
Diagnosing lichen planopilaris involves a combination of clinical evaluation, medical history review, and specialized tests. A dermatologist may perform a scalp biopsy to examine the affected tissue under a microscope. Other tests, such as blood tests or patch testing, may be recommended to rule out other possible causes and triggers. It is essential to consult with a dermatologist experienced in diagnosing and treating lichen planopilaris for accurate results. Early and accurate diagnosis is crucial for implementing an effective treatment plan and managing lichen planopilaris symptoms.
Lichen planopilaris should be distinguished from other causes of scarring hair loss, such as frontal fibrosing alopecia. Non-scarring alopecia areata may resemble early-stage lichen planopilaris but require different treatments. Trichoscopy aids in distinguishing lichen planopilaris from other non-scarring alopecias. Dermatologists may perform blood tests to exclude underlying autoimmune diseases. Examination of the nails and mucous membranes can help differentiate lichen planopilaris from other forms of lichen planus.
Corticosteroids, both oral and topical, are commonly used in the dermatology field to address lichen planopilaris (LPP), a condition characterized by a scarring rash on the scalp. For more severe cases, immunosuppressive agents like mycophenolate mofetil may be prescribed. Additionally, antibiotics can help control any secondary infections associated with LPP. Topical minoxidil has shown efficacy in promoting the regrowth of hair in small affected areas. In cases of permanent hair loss caused by LPP, hair transplantation can be considered.
To treat lichen planopilaris, dermatologists often prescribe corticosteroids such as topical clobetasol propionate to reduce inflammation. Another medication, hydroxychloroquine, can modulate the immune system and help manage this condition. Topical calcineurin inhibitors like tacrolimus can also be used to alleviate inflammation on the scalp. In refractory cases, methotrexate, a systemic immunosuppressive agent, may be recommended. Retinoids like acitretin can normalize the abnormal growth cycle of hair follicles affected by lichen planopilaris. These pharmacological measures have shown efficacy in managing the symptoms of lichen planopilaris.
Protecting the scalp from sun exposure, either by wearing hats or using sunscreen, is an important measure for managing lichen planopilaris. It's also advisable to avoid harsh hair treatments and styling products to minimize scalp irritation. Using gentle shampoos and conditioners can help maintain scalp health in individuals with lichen planopilaris. If bald patches are a concern, wearing wigs or other hairpieces can provide cosmetic coverage.
Since I have worked with many with Lichen Planopilaris, it is my recommendation that you wear a clip-on system instead of an attached hair topper. It is essential to treat your irritated scalp, therefore, an attached hair system may not be advisable. A scalp with Lichen can become crusty, and needs consistent cleaning, and massage. A wig may be too heavy, and uncomfortable. Therefore, a clip-on hair system may work best.
Once your hair loss is under control, see the below video on how we can help on an aesthetic level. All the while giving you access to treating your scalp. At Noelle Salon, you will be working with a team of expert hair loss stylists who understand LLP and will offer our best advice as to how to restore your hair.
Depending on where you are experiencing hair loss, we may use hair extensions which also allows you or your physician to treat your scalp. Soothing creams should be avoided directly on the hair extension attachment.
Living with lichen planopilaris requires long-term management as it is a chronic condition. Regular follow-up appointments with a dermatologist are necessary to monitor the progress of the disease. Support groups and online communities can provide valuable emotional support for individuals dealing with lichen planopilaris. Adhering to the prescribed treatment plan and maintaining scalp hygiene are essential in effectively managing the condition. It is important to maintain a positive outlook and seek professional help when needed to cope with the challenges that arise.
We treat your lichen planopilaris with the utmost compassion, we will also help to soothe your scalp with scalp treatments, and massage prior to applying hair toppers or wigs. Meet us at a free and private consultation . It is never a good idea to glue a hair system onto your head when experiencing hair loss due to Lichen Planopilaris.

Lichen planopilaris typically manifests with distinct clinical features that are vital for diagnosis. Patients often present with smooth, white patches of hair loss on the scalp, where no hair follicle openings are visible. The affected areas may be surrounded by redness and scaling, and it is not uncommon for patients to experience symptoms such as itching, tenderness, and discomfort. The condition is progressive, and small patches may coalesce over time, leading to larger areas of baldness.
Diagnosis is primarily clinical, supported by trichoscopy, which reveals absent hair follicles and other characteristic changes. In cases where the diagnosis remains uncertain, a scalp biopsy might be conducted to confirm the condition. Recognizing these clinical features is essential for timely intervention and to alleviate the psychological distress often associated with hair loss.
Variations in Clinical Features Across Different Skin Types
The clinical presentation of lichen planopilaris remains relatively consistent across diverse skin types, with no significant variations noted. However, the visibility and severity of symptoms may differ based on an individual's skin pigmentation. For instance, in lighter skin tones, the characteristic white patches may be more pronounced, while in darker skin, the affected areas could present with darker pigmentation or even hyperpigmentation.
Skin Type
Clinical Features Observed
Light Skin
Prominent white patches, redness
Dark Skin
Possible hyperpigmentation, less visible patches
Regardless of skin type, the key symptoms—such as itching, redness, and hair loss—remain constant. Understanding these variations helps healthcare providers tailor their approach to diagnosis and treatment, ensuring effective management for all patients, regardless of their skin type.
Complications Associated with Lichen Planopilaris
Lichen planopilaris can lead to several complications, primarily centered around hair loss and its associated psychological effects. Permanent alopecia is the most significant long-term consequence, with some patients experiencing complete loss of hair in affected areas. In more severe cases, loss of eyelashes and eyebrows may occur, further impacting an individual's self-esteem and quality of life.
Additionally, the psychological distress stemming from visible hair loss can lead to anxiety and depression in some patients. Understanding these potential complications is essential for healthcare providers to offer comprehensive care that addresses both the physical and emotional aspects of living with lichen planopilaris. Early intervention and support are crucial in mitigating these long-term effects.
Anyone treat lichen planopilaris with topical steroids only?
Topical steroids can be effective for treating lichen planopilaris (LPP) hair loss, especially in mild cases. They help reduce inflammation and suppress immune responses affecting the scalp. However, treatment effectiveness varies among individuals, and consulting a dermatologist is crucial for a comprehensive and personalized approach to managing LPP.
Diagnosis and Differential Diagnosis of Lichen Planopilaris
The diagnosis of lichen planopilaris begins with a thorough clinical examination and patient history, focusing on the presence of characteristic symptoms. Dermatologists may utilize trichoscopy to identify specific features such as absent hair follicles, white dots, and perifollicular scaling. In some instances, a scalp biopsy may be necessary to confirm the diagnosis, especially when distinguishing it from other types of scarring alopecia.
Differential diagnosis is crucial, as conditions like discoid lupus erythematosus and alopecia areata may present similarly. A comprehensive medical evaluation, including blood tests and examinations of the nails and mucous membranes, can help differentiate lichen planopilaris from these other disorders. Ensuring an accurate diagnosis is vital for implementing an appropriate treatment strategy.
Treatment Options for Lichen Planopilaris
Management of lichen planopilaris is multifaceted, focusing on reducing inflammation and preventing further hair loss. Common treatment options include potent topical corticosteroids, which are often the first line of defense against inflammation. In cases where topical treatments are insufficient, oral medications such as hydroxychloroquine or immunosuppressive agents may be prescribed to manage active disease.
Therapies aimed at promoting hair regrowth, such as topical minoxidil and platelet-rich plasma injections, have also shown promise. It is essential for patients to work closely with their dermatologist to develop a tailored treatment plan that addresses their specific symptoms and progress. Early intervention and consistent management can significantly improve outcomes and enhance the quality of life for those affected by lichen planopilaris.
Non-pharmacological Treatment Approaches
Non-pharmacological treatment approaches for lichen planopilaris emphasize lifestyle changes and supportive measures that can enhance overall well-being and potentially alleviate symptoms. These strategies can be integral for patients seeking to manage their condition effectively. Consider the following:
-
Dietary Adjustments: Incorporating a balanced diet rich in vitamins and minerals may support skin health and immune function. Foods high in omega-3 fatty acids, antioxidants, and vitamins A, C, and E can be beneficial.
-
Stress Management: Utilizing stress reduction techniques such as mindfulness, yoga, or meditation can help mitigate flare-ups associated with emotional trauma.
-
Scalp Care: Gentle cleansing routines and the use of mild hair products can prevent further irritation. Avoiding harsh chemicals and excessive heat styling is also recommended.
Adopting these non-pharmacological treatment approaches can significantly contribute to the management of lichen planopilaris, fostering an environment conducive to healing while complementing pharmacological interventions.
Prognosis and Outcomes for Patients with Lichen Planopilaris
The prognosis for patients with lichen planopilaris varies widely, influenced by factors such as the timing of diagnosis and the effectiveness of treatment. While some individuals may experience spontaneous improvement over time, others may see a progressive worsening of symptoms, leading to permanent hair loss. Long-term effects can include not only physical changes but also psychological impacts, such as reduced self-esteem and anxiety related to visible hair loss.
Outcomes depend heavily on early intervention and adherence to treatment plans. Patients who actively engage in their management and follow dermatologist recommendations often report better results. Understanding the unpredictable nature of lichen planopilaris is crucial for patients and healthcare providers alike, ensuring that appropriate support and resources are available throughout the journey of managing this condition.


